Welcome to the Providers' Hub
EviCore by Evernorth is committed to enhancing the utilization management experience for our providers. That’s why we have the Providers’ Hub, your “one-stop-shop” for resources designed to help you deliver optimal experiences for your patients. See our training materials, clinical guidelines, registration tutorials, contact information, and more.
EviCore is continually working to enhance your prior authorization (PA) experience by streamlining and enhancing our overall PA process. You may notice incremental enhancements to our online interface and case-decision process. Should you have feedback regarding your experience, please provide it in the Web Feedback online form.
EviCore Unified Provider Experience (UPX) - Dashboard Training
Specialty Therapy Provider Portal Overview
Is My Case Urgent?
We're here to help
Live chat is available M-F 7 AM - 7 PM EST
Email: portal.support@evicore.com
Phone: 800-646-0418 option 2
Training Resources
Upload Information
Login to your account at https://www.evicore.com/provider. Select the CareCore National portal and then select authorization lookup and upload additional clinical.
UPLOAD INFORMATION
Create a Case
To login, click the link below to take you to the login page. Please enter your User ID and Password. If you do not have a user ID and Password, click register.
GO TO PROVIDER LOGIN PAGE
How To Register
If you do not have a user ID and password, click register on the login screen. For default portal: select CareCore National.
GO TO PROVIDER REGISTER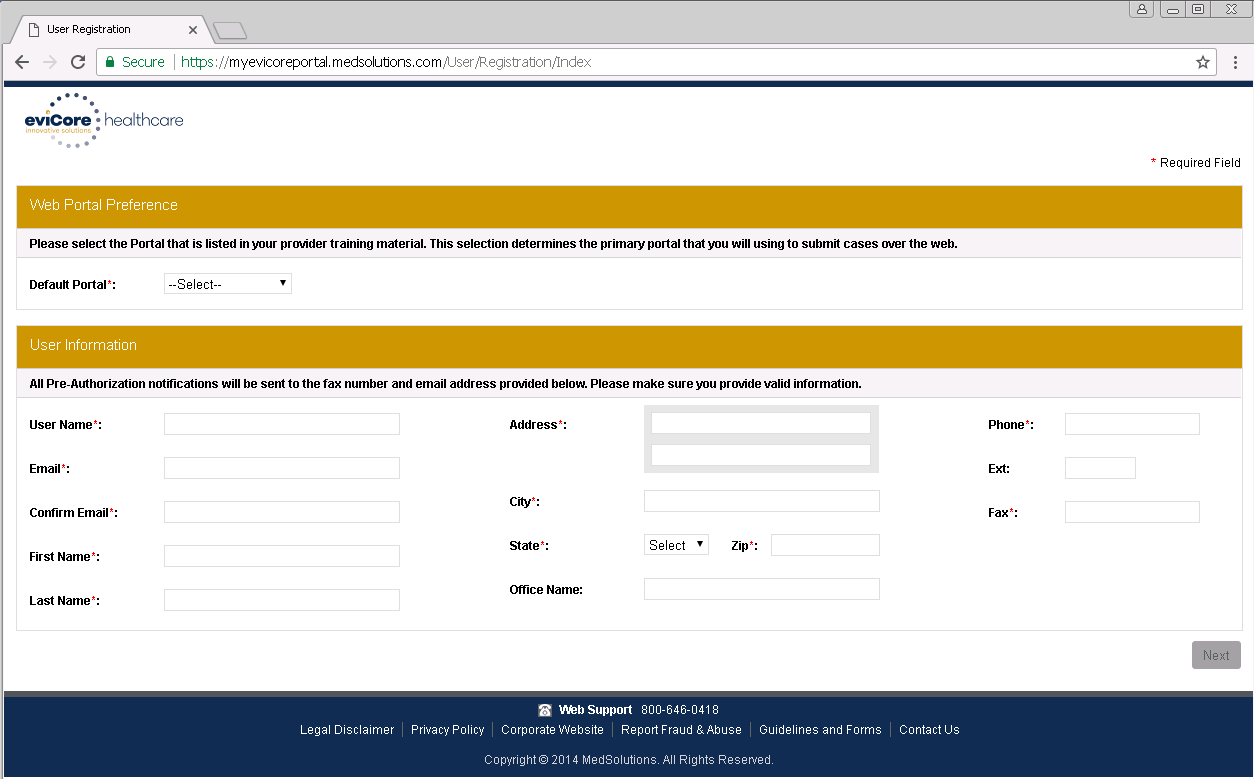
Need Help?
Trouble resetting your password?
